Antimicrobial stewardship in aged care is important to improve the safe and appropriate use of antimicrobials and decrease the risk of antimicrobial resistance for older people.
The Commission is seeking real-world case studies from health service organisations to share experiences of implementing the Comprehensive Care Standard.
The Commission is working in partnership with The George Institute for Global Health and Sepsis Australia to extend the National Sepsis Program. This program aims to improve the awareness, recognition and support for people at risk of or diagnosed with sepsis in Australia.
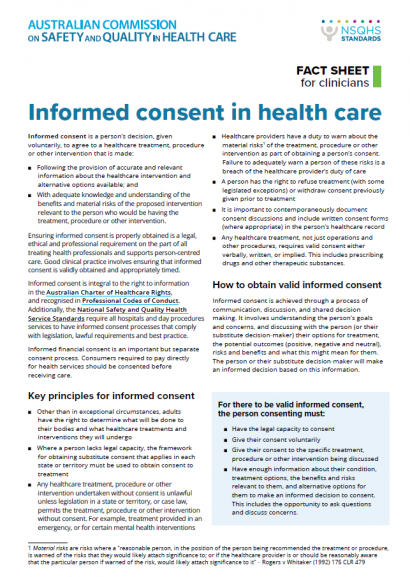
Ensuring informed consent is properly obtained is a legal, ethical and professional requirement on the part of all treating health professionals and supports person-centred care.
The Commission has developed resources for health service organisations (HSOs), accrediting agencies and assessors to support implementation of the safety and quality standards of the National Clinical Trials Governance Framework (NCTGF).
To support implementation of the NSQHS Standards, the Australian Commission on Safety and Quality in Health Care provides guidance for the submission of applications, registrations, requests for extensions and notifications of risk.
The Commission has developed guidance to address all aspects of medicine selection and storage that can affect the likelihood of medication error.
The Australian Commission on Safety and Quality in Health Care convened the Clinical Quality Registries (CQR) Advisory Group, comprising members with relevant expertise and experience in the CQR sector.
Effective management of chronic conditions requires multidisciplinary, coordinated care. Whilst some patients receive this type of care, the current Australian health system does not provide the ideal support for integrated team care. Half of the Australian population has at least one chronic condition, with large variation in the severity and complexity of conditions and the intensity of care patients require.
The Atlas series examines variation in use of some commonly prescribed medicines. Medicines are effective when used appropriately for the right duration. However, substantial variation in use can suggest that some individuals and the community are being exposed to avoidable harms and unnecessary costs, while others may be missing out on an effective treatment.
The range of tests, technologies and treatments that can be used to investigate and manage health problems is growing. Whilst this can bring great benefit, there is an associated risk of diagnosing and treating people for conditions that would never have caused them harm (over-diagnosis).