Clinical handover
A patient who has survived sepsis receives individualised follow-up care to optimise functional outcomes, minimise recurrence, reduce rehospitalisation and manage the ongoing health effects of sepsis. This requires structured, holistic and coordinated post-discharge care and education that involves the patient, their family, carer, general practitioner and other clinicians.
Support and information are provided to the family or carer of a patient who has died from sepsis.
Sepsis is a time-critical medical emergency. Assessment and treatment of a patient with suspected sepsis are started urgently according to a locally approved clinical pathway, and their response to treatment is monitored and reviewed. The patient is reviewed by a clinician experienced in recognising and managing sepsis, and is escalated to a higher level of care when required.
Escalating care
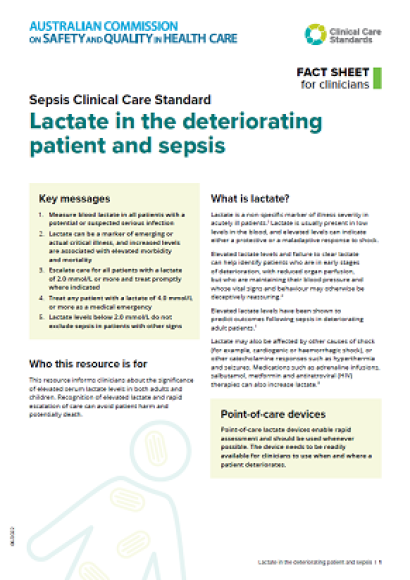
Guidance for clinicians on the seven quality statements from the Sepsis Clinical Care Standard, as well as helpful resources.
Quality statement 1
A patient with any key risk factor for delirium is identified on presentation and a validated tool is used to screen for cognitive impairment, or obtain a current score if they have known cognitive impairment. Before any planned admission, the risk of delirium is assessed and discussed with the patient, to enable an informed decision about the benefits and risks.
Information about the Delirium Clinical Care Standard for clinicians
A diagnosis of sepsis is considered in any patient with an acute illness or clinical deterioration that may be due to infection. A clinical support tool that includes assessment of vital signs and lactate is used to help recognise sepsis early and escalate care when required.
Guidance for clinicians on the eight quality statements from the Low Back Pain Clinical Care Standard, as well as helpful resources.
Guidance for clinicians on the ten quality statements from the COPD Clinical Care Standard, as well as helpful resources.
Escalating care
Appropriate and timely care is provided to patients whose condition is acutely deteriorating.
Information for healthcare services to guide practice and monitor improvement using the clinical care standard, and resources to support implementation.
Based on advice, feedback and discussions with clinical experts and health services from across Australia, the Commission has compiled a list of FAQs and resources that may assist health services in the prevention and reduction of hospital-acquired complications (HACs).
Explore these resources and share your feedback.
Responding to deterioration
The tools and solutions developed through the National Clinical Handover Initiative Pilot Program are available on this page.
Recognising acute deterioration
Resources to support implementation by healthcare services and clinicians including guidance and information, tools, templates, consumer resources, implementation case studies and podcasts.