This page includes resources for implementation of the Preventing and Controlling Infections Standard of the National Safety and Quality Health Service (NSQHS) Standards and National Safety and Quality Primary and Community Healthcare Standards (Primary and Community Healthcare Standards).
The National Pathology Accreditation Advisory Council (NPAAC) is responsible for developing and maintaining the accreditation standards for pathology laboratories in Australia.
Supporting improvements in health care for older people
The Commission supports the safety and quality of health care for older people. This page contains resources that support the delivery of high-quality care of older people across all care settings.
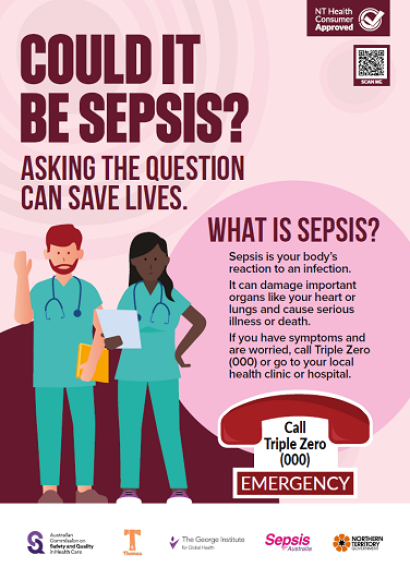
The Commission has developed culturally appropriate resources for Aboriginal and Torres Strait Islander peoples to raise awareness of sepsis.
A reasonable adjustment is a change to an existing approach or process which is essential to ensure a person’s access to a service. Making reasonable adjustment for a person’s disability creates an inclusive environment and facilitates meeting the NSQHS Standards.
Information for healthcare services to guide practice and monitor improvement using the clinical care standard, and resources to support implementation.
The Sepsis Clinical Care Standard describes the health care that should be provided to patients with signs and symptoms of sepsis. It also addresses the care that should be provided in hospital and after discharge, including survivorship.
Guidance for clinicians on the seven quality statements from the Sepsis Clinical Care Standard, as well as helpful resources.
Indicators have been developed to support monitoring of the care recommended in the Sepsis Clinical Care Standard. Clinicians and healthcare services can use the indicators to support local quality improvement activities.
A patient who has survived sepsis receives individualised follow-up care to optimise functional outcomes, minimise recurrence, reduce rehospitalisation and manage the ongoing health effects of sepsis. This requires structured, holistic and coordinated post-discharge care and education that involves the patient, their family, carer, general practitioner and other clinicians.
Support and information are provided to the family or carer of a patient who has died from sepsis.
A patient with known or suspected sepsis has a documented clinical handover at transitions of care. This includes the provisional sepsis diagnosis, comorbidities, and the management plan for medicines and medical conditions. This information is provided to the patient, their family and carer as appropriate.
A patient, their family or carer is informed about sepsis from the time that it is suspected in a way that they can understand. Information includes the expected treatment and potential health effects of sepsis. Information is provided verbally and in writing.
The Sepsis Clinical Care Standard includes seven quality statements describing the key components of care that a patient presenting with signs and symptoms of sepsis should receive so that the risk of death or ongoing morbidity is reduced.