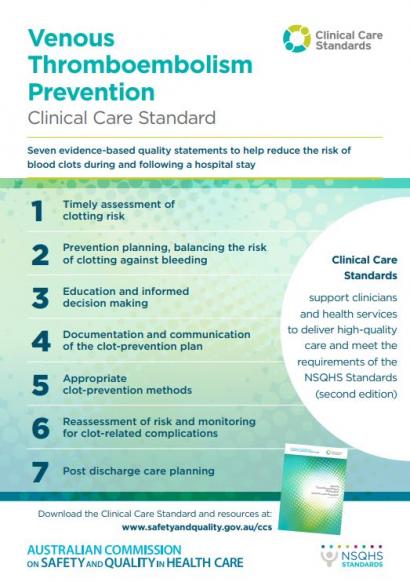
Venous Thromboembolism Prevention Clinical Care Standard
The Venous Thromboembolism Prevention Clinical Care Standard has been developed by the Commission to support clinicians and health services implement the delivery of high-quality care to prevent venous thromboembolism (VTE) acquired in hospital and following hospital discharge.
Introduction
Venous thromboembolism (VTE) is a major cause of morbidity and mortality for patients admitted to hospital, and a common preventable cause of in-hospital death. It is estimated to account for 7% of all deaths in Australian hospitals, and the consequence of developing VTE has been estimated to cost the Australian health system $1.72 billion annually.1
Despite the availability of international evidence-based best-practice guidelines for the prevention of VTE, data from Australia and internationally2-4 suggests that a significant proportion of patients at risk of VTE do not receive care as recommended in current guidelines.
Download the Standard
This resource provides guidance to consumers, clinicians and health services on the care recommended to prevent VTE in hospital and following hospital discharge.
The Venous Thromboembolism Prevention Clinical Care Standard has been endorsed by 12 key professional organisations and colleges including the Thrombosis & Haemostasis Society of Australia and New Zealand (THANZ), the Royal Australasian College of Surgeons (RACS), the Australian Orthopaedic Association (AOA), and the Australian College for Emergency Medicine (ACEM).
Implementing clinical care standards helps health service organisations to meet the requirements of the National Safety and Quality Health Service (NSQHS) Standards for accreditation.
Guide for implementing the VTE Prevention Clinical Care Standard
The Commission has developed a guide to support the implementation of the Venous Thromboembolism Prevention Clinical Care Standard. The Implementation Guide: Venous Thromboembolism Prevention Clinical Care Standard provides a range of strategies, recommendations and case studies, as a starting point for clinicians and health service organisations implementing the clinical care standard.
What is venous thromboembolism (VTE)?
Venous thromboembolism (VTE) is a disease process that includes deep vein thrombosis (DVT) and pulmonary embolism (PE).
| Deep vein thrombosis (DVT) | Occurs when blood clots form in veins, usually deep inside the legs or in the pelvis, where they may cause symptoms like pain, tenderness, redness, or swelling of the leg. |
|---|---|
| Pulmonary embolism (PE) | Occurs when a blood clot breaks off and moves through the veins to block blood vessels in the lungs. This may cause symptoms like shortness of breath, coughing up blood, chest pain, faintness, and loss of consciousness. If the clot blocks enough blood vessels in the lungs, the person can die.5 |
Quality statements
Implementation resources
Use these resources to implement and promote the Venous Thromboembolism Prevention Clinical Care Standard to health services, clinicians, patients and their carers.
Indicator specifications
This resource provides a set of suggested indicators to assist with local implementation of the Venous Thromboembolism Prevention Clinical Care Standard. Clinicians and health services can use the indicators to monitor implementation of the quality statements, and support improvements as needed.
The indicator specification is available from METeOR.
Background information
Despite current efforts, evidence suggests that a large proportion of hospitalised patients are at risk of VTE, however many patients do not receive appropriate VTE prophylaxis.6,7 VTE prevention strategies have been shown to significantly reduce the incidence of VTE by about 70%.
While the incidence of VTE among hospitalised patients is 100 times greater than in the community8, the risk of developing VTE also continues after discharge from hospital. Hospitalisation is a major risk factor for VTE, with about 74% of VTE cases occurring up to three months after hospital discharge.9
The key clinical guideline in Australia for VTE prevention in hospitalised patients was rescinded in 2016.5 The development of the Venous Thromboembolism Prevention Clinical Care Standard was proposed by states and territory health departments as a way of improving the uptake of appropriate VTE prophylaxis strategies.
References
- Access Economics Pty Ltd for the Australia and New Zealand working party on the management and prevention of venous thromboembolism. The burden of venous thromboembolism in Australia, 1 May 2008. Access Economics Pty Ltd; 2008.
- Cohen AT, Tapson VF, Bergmann J-F,Goldhaber SZ, Kakkar AK, Deslandes B, et al.Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet. 2008;371(9610):387–94.
- Kahn SR, Panju A, Geerts W, Pineo GF, Desjardins L, Turpie AG, et al. Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb Res. 2007;119(2):145–55.
- Tapson VF, Decousus H, Pini M, Chong BH, Froehlich JB, Monreal M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest. 2007;132(3):936–45.
- National Health and Medical Research Council. Clinical practice guidelines for the prevention of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to Australian hospitals (rescinded 2016). Melbourne: NHMRC; 2009.
- Assareh H, Chen J, Ou L, Hillman K, Flabouris A. Incidences and variations of hospital acquired venous thromboembolism in Australian hospitals: a population-based study. BMC Health Services Research. 2016;16:511.
- Cohen A, Tapson V, Bergmann J-F, Goldhaber S et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. The Lancet. 2008; 371:387-394.
- Heit JA, Melton LJ, III, Lohse CM, Petterson TM, Silverstein MD, Mohr DN, et al. Incidence of venous thromboembolism in hospitalized patients vs community residents. Mayo Clinic Proceedings. 2001.76(11):1102-10.
- Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Archives of Internal Medicine. 2007;167(14):1471-5.
Contact us
If you have questions about this clinical care standard, please email ccs@safetyandquality.gov.au.
For future updates on standards due to be launched and out for consultation, follow us on X (Twitter) @ACSQHC or subscribe to our eNewsletters.