Information for clinicians - Acute Anaphylaxis Clinical Care Standard
Guidance for clinicians on the six evidence-based quality statements from the clinical care standard, as well as helpful resources.
What do clinicians need to know?
The Acute Anaphylaxis Clinical Care Standard includes six evidence-based quality statements to improve the recognition of anaphylaxis, and the provision of appropriate treatment and follow-up care. The quality statements describe the expected standard for key components of patient care.
Quality Statements
Resources for Clinicians
The following resources have been developed to support the Acute Anaphlylaxis Clinical Care Standard.
The Commission also has a suite of promotional resources to assist in implementation through each Health Service Organisation.
-
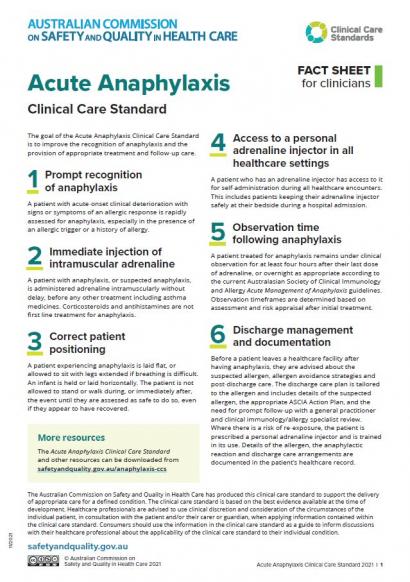
2021Fact sheet
Healthcare professionals can use this fact sheet as a quick summary of the Acute Anaphylaxis Clinical Care Standard.
-
2021Standard
The Acute Anaphylaxis Clinical Care Standard contains six quality statements and a set of indicators to improve the recognition, treatment and follow-up of anaphylaxis in acute care.
-
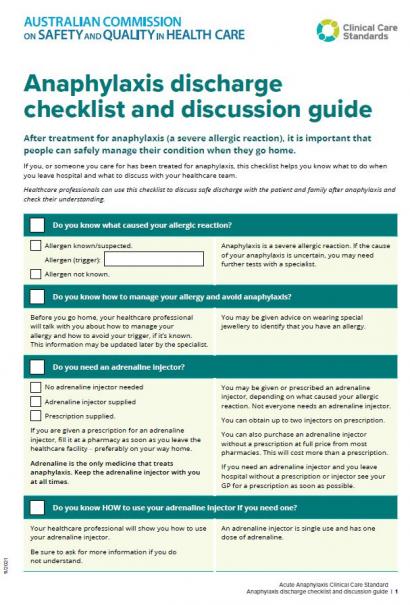
2021Guide, user guide or guidelines
This document provides a discussion guide and checklist to ensure patients who have experienced anaphylaxis are safely discharged from care.
-
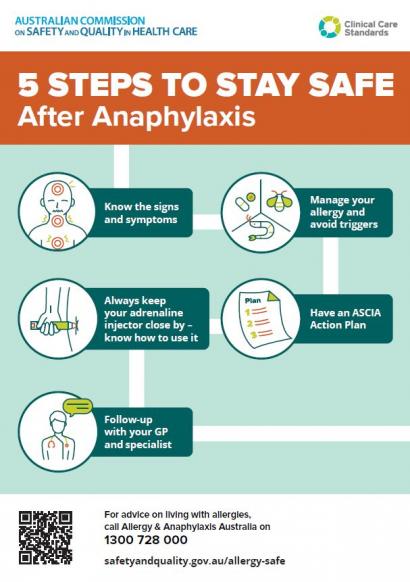
2021Fact sheet
This poster can be used in waiting rooms to inform patients and their families the key messages after experiencing anaphylaxis.
-
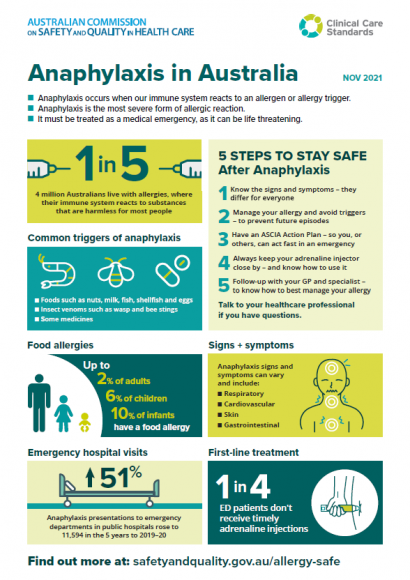
2021Poster or infographic
The Acute Anaphylaxis Clinical Care Standard will help to ensure that Australians receive prompt treatment to manage severe allergic reactions, and that there is continuity of patient care across healthcare settings.
This infographic outlines key data highlights on anaphylaxis in Australia, to support the release of the new standard on 24 November 2021.