- Home
- Standards
- Clinical Care Standards
- Colonoscopy Clinical Care Standard
- Information for clinicians
Information for clinicians – Colonoscopy Clinical Care Standard
Guidance for clinicians on the nine quality statements from the Colonoscopy Clinical Care Standard, as well as helpful resources.
What clinicians need to know
The Colonoscopy Clinical Care Standard contains nine quality statements. It covers the period from when a patient is referred for consideration of colonoscopy through to discharge, including planning for follow‑up care.
A set of indicators is provided to support clinicians and healthcare services to monitor how well they are implementing the care recommended in this clinical care standard and to support local quality improvement activities.
What the standard means for clinicians
What the standard says
When a patient is referred for consideration of colonoscopy, the referring clinician provides sufficient information for the receiving clinician to assess the appropriateness, risk and urgency of consultation. The receiving clinician or service allocates the patient an appointment according to their clinical needs.
What this means for clinicians
Clinicians making referrals
When referring patients for consideration of colonoscopy, provide a comprehensive referral to enable accurate assessment of the patient’s suitability for, and urgency of, colonoscopy. Standard (electronic) templates can help. See the Commission’s Colonoscopy Referral Information for further information, and refer to local HealthPathways where relevant. The referral should include:
- The indication for the referral, including presenting symptoms and the clinical concern
- Results and dates of previous investigations, including iFOBT (indicating whether this was through the National Screening Program), colonoscopies and histopathology
- All relevant medical and family history, including of bowel and other cancers and known genetic predispositions
- Current medicines and other medical conditions
- Previous relevant treatment.
Consider the indications and surveillance intervals recommended in current evidence-based guidelines such as the Cancer Council Australia’s Clinical practice guidelines for the prevention, early detection and management of colorectal cancer, and Clinical practice guidelines for surveillance colonoscopy. Evaluate the likelihood of the patient benefiting from the procedure, considering their overall health, comorbidities, likelihood of benefit from future management, the procedural risk and their willingness to proceed. Discuss with the patient whether the specialist receiving the referral will assess them individually before undertaking the colonoscopy. Give the patient information about what to expect, including whether there are likely to be costs. Provide an opportunity to ask questions and have them answered.
If referral to open-access services is an option, ensure the patient is suitable according to the local service intake guidelines and considering the patient’s age, general health, comorbidities and ability to take bowel preparation independently. Provide clear instructions to the patient on what they need to do to act on the referral, the degree of urgency, and what to do if they cannot get an appointment in the recommended timeframe.
Clinicians receiving referrals
When receiving referrals for colonoscopy, ensure that your protocols and processes allow for reviewing and determining appropriateness for the referral, and for allocating appointments based on clinical need. Clearly communicate the required referral information to referring clinicians, preferably using a standardised template.
What the standard says
A patient is offered timely colonoscopy when appropriate for the investigation of signs or symptoms of bowel disease, surveillance or screening, as consistent with national evidence-based guidelines. Decisions are made in the context of the patient’s ability to tolerate the bowel preparation and colonoscopy, and their likelihood of benefit. If colonoscopy is not appropriate, the receiving clinician advises the patient and their referring clinician of alternative recommended management.
What this means for clinicians
Consider whether colonoscopy is indicated for the patient according to national evidence-based guidelines, the epidemiology of disease (including bowel cancer and inflammatory bowel disease) and how findings on colonoscopy are likely to influence management. Assess the likely benefits to the patient, as well as the risks associated with the bowel preparation, sedation, the procedure itself, any further management and the risks associated with not having the procedure.
Refer to Cancer Council Australia’s Clinical practice guidelines for the prevention, early detection and management of colorectal cancer:
- For people with symptoms suggestive of bowel cancer or a positive iFOBT
- For people who are at markedly higher than average risk for bowel cancer such as those with familial syndromes, where screening colonoscopy is recommended.
For people requiring surveillance colonoscopy (including for inflammatory bowel disease), refer to Cancer Council Australia’s Clinical practice guidelines for surveillance colonoscopy regarding the frequency and surveillance intervals for colonoscopy in high‑risk individuals.
Ensure that colonoscopy is triaged and scheduled according to relevant and locally approved triage criteria, that reflect Cancer Council Australia’s guidelines. If colonoscopy is not appropriate, advise the patient and their referring clinician about recommended alternative diagnostic strategies or management.
What the standard says
Before starting bowel preparation, a patient receives comprehensive patient‑appropriate information about bowel preparation, the colonoscopy, and sedation or anaesthesia. The patient has an opportunity to discuss the reason for the colonoscopy, the risks, benefits, financial costs and alternative options before deciding to proceed. Their understanding is assessed, and the information provided and their consent to sedation, colonoscopy and therapeutic intervention is documented.
What this means for clinicians
Provide the patient (or their responsible decision maker where relevant) with clear and comprehensive information about all aspects of the colonoscopy relevant to the patient’s decision and consent. Include information about the bowel preparation, the use of sedation (or anaesthesia), the colonoscopy and any therapeutic interventions. Use language that they can understand. Arrange an interpreter if required.
Inform the patient of:
- The reason for the colonoscopy
- Its likelihood of benefits
- Potential adverse events, including those related to the bowel preparation or sedation, perforation, bleeding (immediate and delayed), splenic injury and missed pathology
- What happens during a colonoscopy
- The financial costs
- The alternatives to having the colonoscopy, including any risks of not having the colonoscopy.
Information on potential adverse events, risks and benefits should be individualised and relevant to the patient. Provide adequate time for the patient to consider the information provided and to ask questions before consenting. Respect the patient’s decision and document it and their informed consent in the medical record, with a description of the information discussed and provided to the patient.
What the standard says
A patient booked for colonoscopy receives a bowel preparation product and dosing regimen individualised to their needs, comorbidities, regular medicines and previous response to bowel preparation. The importance of good bowel preparation for a quality colonoscopy is discussed with the patient. They are provided with consumer-appropriate instructions on how to use the bowel preparation product and their understanding is confirmed.
What this means for clinicians
Provide written and verbal consumer-appropriate information to patients preparing for colonoscopy, using interpreter services where necessary. Select an appropriate bowel preparation agent and ensure the patient knows how to obtain and use it, considering individual risks, comorbidities, current medicines, and the patient’s previous experience with bowel-cleansing medicines. Clearly explain the purpose of bowel preparation, the importance of following the prescribed procedure, the regimen and the potential side effects of the bowel preparation products. Allow the patient appropriate time to ask questions and confirm that they understand what to do and its importance. Let the patient know who they can contact if they are unclear about what to do.
A split-dose regimen results in a higher quality colonoscopy examination compared with ingestion of the entire preparation on the day or evening before the colonoscopy and has been associated with increased adenoma detection rates. Typically, this involves splitting the standard dose of the bowel preparation between the day before and the morning of the colonoscopy. Ensure that some of the bowel preparation dose is given on the same day of the procedure (3–6 hours before the planned start of the procedure).
Ensure patients on diabetes medicines, anticoagulants, antiplatelets, or other medicines are provided with individualised instructions about how to adjust their medicines and manage their condition as they undergo bowel preparation. Enquire about the patient’s use of medicines to lose weight, due to the potential complications in endoscopic procedures (see Related resources for further information). Consider whether a patient with relevant comorbidities needs specific health or personal support while undergoing bowel preparation. For example, overnight admission for patients who are unlikely to manage bowel preparation independently.
What the standard says
Before colonoscopy, a patient is assessed by an appropriately trained clinician to identify any increased risk, including cardiovascular, respiratory or airway compromise. The use of sedation is planned accordingly. The risks and benefits of sedation are discussed with the patient. Sedation is administered and the patient is monitored throughout the colonoscopy and recovery period in accordance with Australian and New Zealand College of Anaesthetists guidelines.
What this means for clinicians
Provide patients with the opportunity to discuss the approach to sedation. This may include the option of no sedation where this is the patient’s preference and is clinically appropriate.
Ensure that the patient’s suitability for sedation is assessed in advance of the colonoscopy by a clinician who is appropriately trained to make such an assessment. This should include assessment of any increased risks such as cardiovascular, respiratory or airway compromise.
Ensure that the facility is appropriate for the patient, taking into account their clinical requirements and comorbidities, as described in ANZCA’s Guideline for the perioperative care of patients selected for day stay procedures (PG15). If an increased risk is identified, an anaesthetist, or other trained and credentialed medical practitioner within their scope of practice, should assess the patient and be present during the colonoscopy to care for the patient.
Consider whether the patient is likely to require overnight admission or increased medical support and whether admission to a day procedure unit is appropriate. The sedationist should discuss the risks and benefits with the patient and obtain their informed decision and consent. Ensure that the patient understands that their awareness of the colonoscopy will depend upon the depth of sedation.
Sedation must be administered by a credentialed practitioner working within their scope of practice. Both anaesthetist and non-anaesthetist clinicians should provide sedation as described in current ANZCA guidelines with respect to:
- The number of staff present during the sedation and their level of training, competence and scope of clinical practice
- Facilities, equipment and medicines
- Administration of sedation
- Monitoring of patients during the colonoscopy and in the recovery room.
Note: Whilst anaesthetists are specialists in the sedation–anaesthesia continuum, sedation may be administered and managed by clinicians from other clinical disciplines. ANZCA’s Guideline on procedural sedation (PG09) outlines the requirements for non-anaesthetist sedationists managing minimal or moderate procedural sedation. (See sedationist in the Glossary for further information). For anaesthetists targeting deep sedation or general anaesthesia, the patient should be managed by a medical practitioner trained and credentialed to provide anaesthesia. Refer to ANZCA’s Guideline for the perioperative care of patients selected for day stay procedures (PG15) and Position statement on roles in anaesthesia and perioperative care (PS59[A]).
What the standard says
A patient’s colonoscopy is performed by a credentialed clinician working within their scope of clinical practice, who meets the requirements of an accepted certification and recertification process. Sedation or anaesthesia, and clinical support are provided by credentialed clinicians working within their scope of clinical practice.
What this means for clinicians
Ensure that your training, skills and experience allow you to provide safe, high‑quality care to a patient undergoing colonoscopy, in accordance with expected professional standards. Comply with your health service organisation’s policies and procedures regarding your scope of clinical practice. Interact with your peers to ensure your performance, and theirs, meets the accepted requirements for safety and quality (for example, participate in peer-review meetings and quality clinical improvement processes – including the collection of quality indicators and reviews of evidence-based best practice).
If you are a colonoscopist, undergo certification and participate in a recertification process that is accepted by your professional association and employer. Supervise trainees at a level appropriate to their skill and experience.
If you are a clinician providing sedation, ensure you meet the Safe Sedation Competencies as described in ANZCA’s Guideline on procedural sedation (PG09).
What the standard says
When a patient is undergoing colonoscopy their entire colon – including the caecum – is examined carefully and systematically. The adequacy of bowel preparation, clinical findings, biopsies, polyps removed, therapeutic interventions and details of any adverse events are documented. All polyps removed are submitted for histological examination.
What this means for clinicians
To maximise adenoma detection, intubate the caecum or terminal ileum and allow adequate time for mucosal inspection whenever performing colonoscopy. In people with previous resection, examine the remaining bowel thoroughly. Assess the adequacy of bowel preparation using a validated tool such as the Boston Bowel Preparation Scale, Ottawa Bowel Preparation Scale, or the Aronchick Scale.
Document the quality of the bowel preparation, whether caecal intubation was achieved (with photodocumentation), withdrawal time, clinical findings, the details of polyps removed, how they were removed and whether they were retrieved. Ensure that all polyps removed are retrieved, where possible, and are sent for histopathology examination. For patients referred for colonoscopy due to a positive National Screening Program iFOBT result, reporting to the National Cancer Screening Register should occur as soon as possible.
Record adverse events, including perforation, post‑polypectomy bleeding and sedation-related cardio-respiratory compromise in the patient record and relevant quality systems (for example, the facility’s incident monitoring system). Inform the patient if adverse events have occurred and how they have been managed.
Equipment used to perform the colonoscopy should be of adequate quality to enable safe and accurate visualisation and photodocumentation of the bowel. Any adjunctive technologies (such as artificial intelligence [AI] polyp detection, foot pump irrigation and narrow band imaging) should be used in an assistive capacity and according to local policy. Clinicians remain accountable for delivering safe and high‑quality care regardless of the technology used, and for ensuring their practice meets their professional obligations.
What the standard says
Following recovery and before discharge, the patient is advised verbally and in writing about the preliminary outcomes of the colonoscopy, the nature of any therapeutic interventions or adverse events, when to resume regular activities and medicines, and arrangements for medical follow‑up. The patient is safely discharged into the care of a responsible adult, in accordance with Australian and New Zealand College of Anaesthetists guidelines.
What this means for clinicians
Before discharge, the responsible clinician or their delegate should talk to the patient and briefly describe what happened during the colonoscopy. This includes whether the colonoscopy was completed satisfactorily, initial observations, whether biopsies or polypectomies were performed, and if any adverse events occurred. Advise patients of any arrangements for follow‑up medical consultation and when final results and recommendations will be provided to them and their referring clinician.
Ensure patients are discharged by authorised clinical personnel into the care of a responsible adult after satisfactory discharge criteria are met. If, despite all reasonable efforts, a responsible adult is not available, the clinician responsible for managing sedation may exercise their judgement in deciding alternative post‑sedation supervision and transport (excluding driving or public transport). Any exception should take into account the nature and duration of the sedation, and the patient’s recovery and risk of adverse events, in accordance with ANZCA’s Guideline on procedural sedation (PG09). Alternatives, including admission or scheduling of appointments to allow longer periods in recovery, should be explored when scheduling admissions to avoid denying colonoscopy to people due to their social circumstances.
Provide instructions about early post‑procedure care and resumption of normal activities, including making legally binding decisions, operating machinery and resuming regular medication. Advise patients of what to do if they experience symptoms suggesting a complication of the colonoscopy and provide them with specific contact details for obtaining appropriate advice. Any information given verbally about the procedure or post‑discharge should also be provided in written format. Consider admission for a patient at high risk of an adverse outcome who is otherwise not suitable for discharge.
What the standard says
The colonoscopist communicates the reason for the colonoscopy, its findings, any histology results and recommendations for follow‑up in writing to the general practitioner, any other relevant clinician and the patient. This information is recorded in the facility records and other electronic shared record management systems to enable accurate follow‑up by other clinicians. Recommendations for surveillance colonoscopy, if required, align with national evidence-based guidelines. If more immediate treatment or follow‑up is needed, the colonoscopist makes appropriate arrangements.
What this means for clinicians
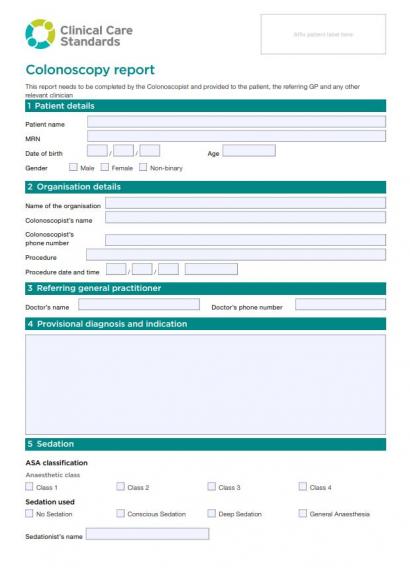
Ensure a colonoscopy report is provided to the patient, their GP and any other relevant clinicians that includes:
- The reason for the colonoscopy
- Findings during the colonoscopy examination
- Histology results where relevant
- Recommendations for follow‑up based on national evidence-based guidelines.
Ensure that both positive and negative histology findings are communicated. The need and time interval for future screening and surveillance colonoscopies should be guided by evidence-based guidelines, such as the Cancer Council Australia’s Clinical practice guidelines for the prevention, early detection and management of colorectal cancer, and Clinical practice guidelines for surveillance colonoscopy. If prompt treatment or investigation is required (such as for histologically confirmed colorectal cancer or high‑risk lesions), make the necessary arrangements and ensure these are communicated to the patient and their referring clinician. If presenting symptoms have not been explained by the colonoscopy, advise the patient and refer on if further investigation or treatment is required.
Upload the report and results to the patient’s healthcare record and My Health Record (if this capability is available in clinical information systems). For National Screening Program participants, report colonoscopy outcomes, results and adverse events to the National Cancer Screening Register.
Resources
The resources below have been developed to support clinicians to implement the care described in the standard. Also see our full set of implementation resources including resources for healthcare services, and consumers, and other related resources relevant to the standard.
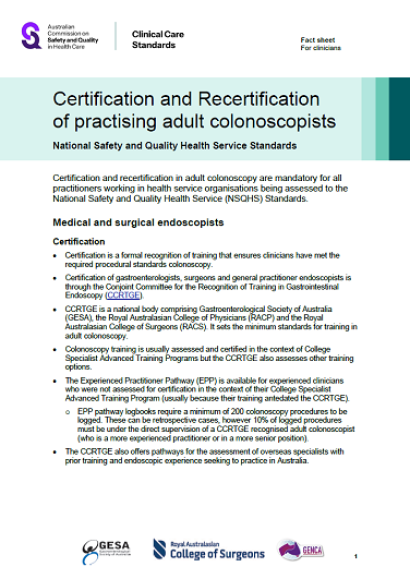
Credentialing, certification and re-certification of colonoscopists
Certification (of training) and recertification (of ongoing competency) in adult colonoscopy are mandatory for all practitioners working in health service organisations being assessed to the National Safety and Quality Health Service Standards (second edition). Download the following fact sheet for information for clinicians on certification and re-certification.
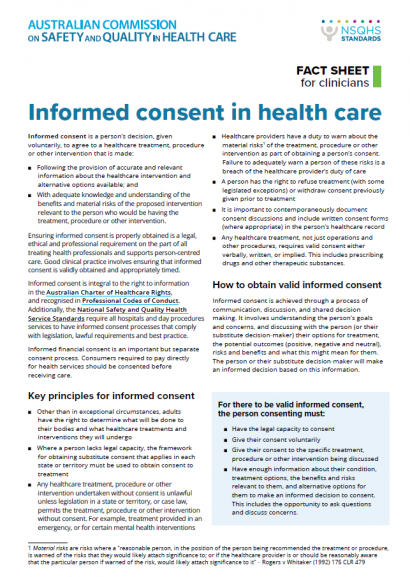
Informed consent for colonoscopy
Quality statement 3 in the clinical care standard states that a patient should receive adequate information and provide informed consent before starting bowel preparation. Find out what informed consent means for colonoscopists.
Templates for referral, reporting and follow-up letters
Templates have been developed to assist clinicians to draft referral, reporting and follow-up letters.