Information for clinicians – Low Back Pain Clinical Care Standard
Guidance for clinicians on the eight quality statements from the Low Back Pain Clinical Care Standard, as well as helpful resources.
What clinicians need to know
The Low Back Pain Clinical Care Standard includes eight evidence-based quality statements to improve the early assessment, management, and review and referral of patients with low back pain, and to improve shared decision making about which tests and treatments are most effective in managing low back pain.
A set of indicators is provided to support clinicians and healthcare services to monitor how well they are implementing the care recommended in this clinical care standard and to support local quality improvement activities.
What the quality statements mean for clinicians
Resources for clinicians
The resources below have been developed specifically for clinicians.
You can also see our full list of implementation resources including guidance for healthcare services and resources for consumers.
-
2022Standard
The Low Back Pain Clinical Care Standard contains eight quality statements and eleven indicators to improve the early assessment, management, and review and referral of patients with low back pain.
-
2022Fact sheet
Lists the eight quality statements in the Low Back Pain Clinical Care Standard and describes what each statement means for clinicians assessing and managing people with low back pain.
-
2022Fact sheet
An overview of the care described in the clinical care standard, with key actions and communication tips for general practitioners.
-
2022Fact sheet
An overview of the care described in the clinical care standard, with key actions and communication tips for emergency department physicians.
-
2023Fact sheet
This resource provides an evidence-based approach to the early assessment, management, review and referral of patients with low back pain, who present with a new acute episode. The guide includes simple guidance and communication tips for physiotherapists.
-
2023Fact sheet
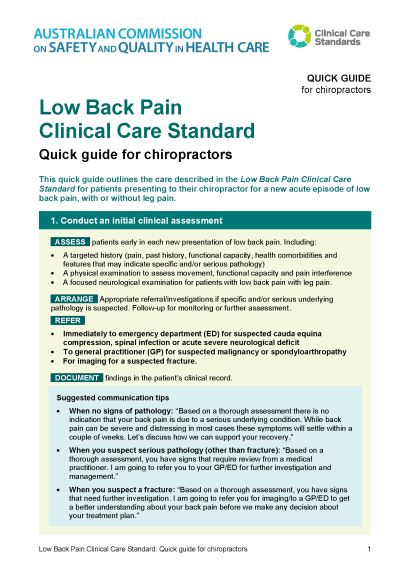
This quick guide outlines the care described in the Low Back Pain Clinical Care Standard for patients presenting to their chiropractor for a new acute episode of low back pain, with or without leg pain.