Information for clinicians – Third and Fourth Degree Perineal Tears Clinical Care Standard
Information about the Third and Fourth Degree Perineal Tears Clinical Care Standard and resources for clinicians.
What do clinicians need to know?
The Third and Fourth Degree Perineal Tears Clinical Care Standard provides guidance to clinicians to support high-quality, evidence-based care. It also provides information to guide discussions between clinicians and women about third and fourth degree perineal tears, in order to support shared decision making and informed consent.
Quality statements
Resources for clinicians - information and videos
A number of resources have been developed to support the Third and Fourth Degree Perineal Tears Clinical Care Standard.
Resources designed specifically for clinicians are available below.
Webcast launch – video recording
The Commission hosted a webcast to launch the standard on 21 April 2021.
The launch and panel discussion hosted by Professor Anne Duggan, Acting Chief Medical Officer, provides an overview of the new standard, and discusses some of the evidence driving the need for change.
Expert panellists include obstetrician Associate Professor Emmanuel Karantanis, midwifery expert Professor Hannah Dahlen, physiotherapist Natalie McConochie, and Janelle Gullan, a woman who experienced a third-degree perineal tear.
Talking about Tears - a video for clinicians
Midwifery and obstetrics experts, and women with experience of perineal tears discuss how to talk about perineal tears - and why it is so important to do so.
-
2021Standard
This complete version of the clinical care standard includes information about using clinical care standards and the background to the development of the Third and Fourth Degree Perineal Tears Clinical Care Standard. It provides descriptions of what each quality statement means for women, clinicians, and health service organisations, as well as indicators for local monitoring and supporting evidence.
-
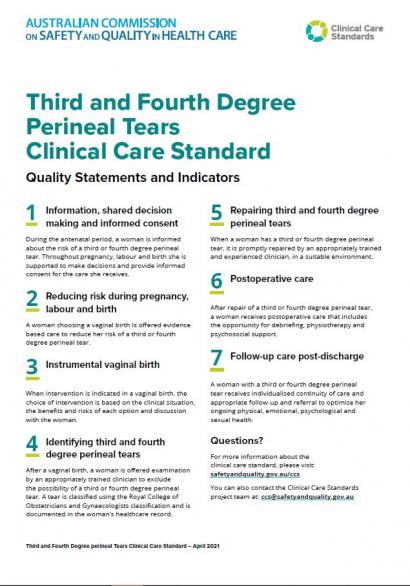
2021Fact sheet
A one page list of all the quality statements and indicators included in the Third and Fourth Degree Perineal Tears Clinical Care Standard.
-
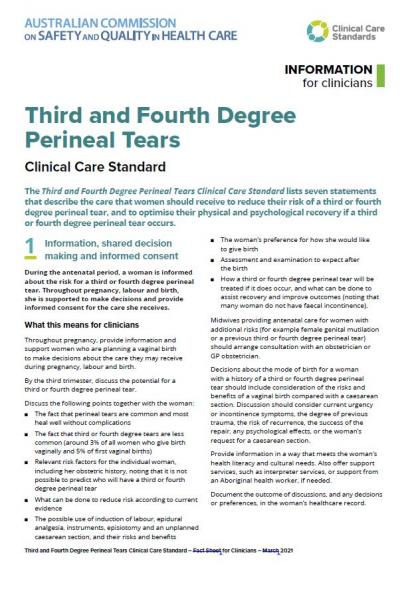
2021Fact sheet
This document describes each of the quality statements and indicators included in the Third and Fourth Degree Perineal Tears Clinical Care Standard for clinicians involved in the care of women during pregnancy, labour and birth, and after a tear.
-
2021Presentation
The webcast slides were part of the presentation shown at the launch of the Third and Fourth Degree Perineal Tears Clinical Care Standard on 21 April 2021. These slides can be used for presentations and training. A video of the launch webcast can be viewed on the Third and Fourth Degree Perineal Tears Clinical Care Standard web page.
Information resources for women
A number of resources have also been developed specifically for women. They can also be used by clinicians when discussing perineal tears with women.
Third and fourth degree tears during labour and birth – a video for women
-
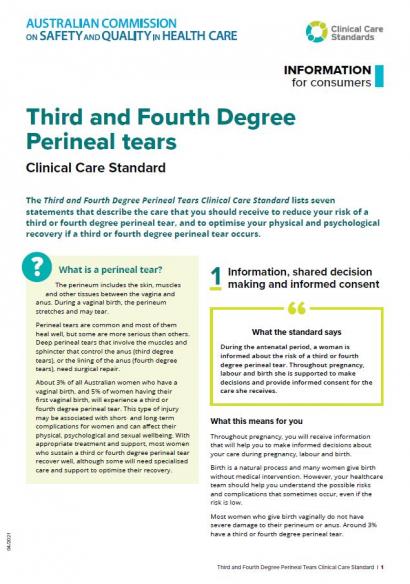
2021Fact sheet
This document describes each of the seven quality statements in this clinical care standard and what they mean for women.
-
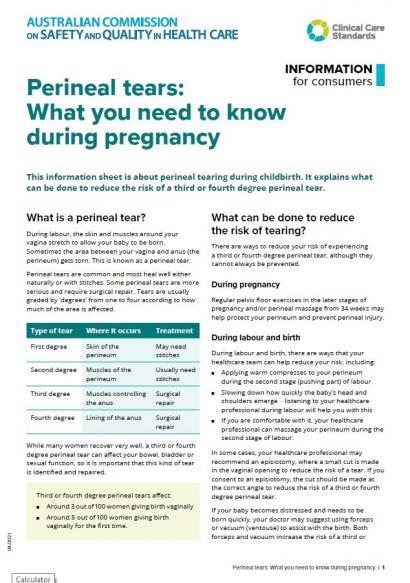
2021Fact sheet
This information sheet for women is about perineal tearing during childbirth. It explains what can be done to reduce the risk of a third or fourth degree perineal tear.
-
2021Fact sheet
If you have a third or fourth degree perineal tear during childbirth, this information sheet will help you understand the treatment and follow-up care you should receive to support your recovery.